Heat Stroke and Asbestos Abatement Workers: A Critical 5-Minute Briefing
- OliveHealth

- Apr 8
- 4 min read
By: Edwin Fuentes MD

Today, I want to address a serious and potentially life-threatening condition: heat stroke, with a specific focus on its dangers for asbestos abatement workers. Given the nature of this work, asbestos abatement workers face a unique combination of risk factors that demand our utmost attention and proactive measures.
BACKGROUND
In 2023, there were nearly 120,605 heat-related emergency department (ED) visits recorded in the CDC's ESSENCE system. Here's a more detailed breakdown:
Total Visits: A total of 120,605 heat-related emergency department visits were recorded in the CDC's ESSENCE system from January 1 to December 31, 2023.
Heat-related deaths: A study published in the American Medical Association journal JAMA found that 2,325 people died from heat in 2023, which researchers admit is likely an undercount.
Time of Year: Over 90% of these visits occurred during the warm-season months of May to September.
Geographic Distribution: The highest rates of heat-related visits were experienced in a region encompassing Arkansas, Louisiana, New Mexico, Oklahoma, and Texas.
Record-High Rates:In 2023, all regions of the US experienced at least one day where the rate of heat-related emergency department visits reached an extreme level, topping 95% of rates from 2018 to 2022.
Increased Visits:These heat-related ER visits were a notable increase from the prior average of around 60,000-80,000 annually.
SIGNS AND SYMPTOMS
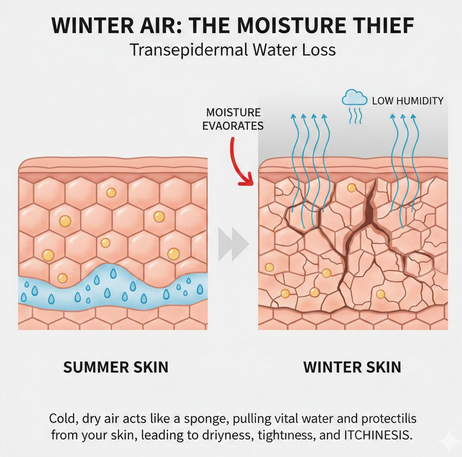
Heat stroke is a medical emergency characterized by a dangerously elevated core body temperature, typically above 104 degrees Fahrenheit (40 degrees Celsius), coupled with neurological dysfunction. Understanding the pathophysiology of heat stroke is crucial. Our bodies normally regulate temperature through mechanisms like sweating. However, in extreme heat or during intense physical exertion, especially when coupled with dehydration, these mechanisms can fail. This leads to a rapid rise in core temperature, causing cellular damage throughout the body. The brain, heart, kidneys, and liver are particularly vulnerable.
This can result in
confusion,
disorientation,
seizures,
and ultimately, coma
and death if not treated immediately.
THE ASBESTOS ABATEMENT WORKER
Now, let's consider the specific risks faced by asbestos abatement workers. The very nature of your job creates a perfect storm for heat stroke. You are often working in enclosed abatement locations with lack of air circulation, compounding the ambient heat.
The vigorous physical labor required for asbestos removal generates significant internal body heat. Furthermore, the mandatory use of
the Tyvek suits, while essential for protection against asbestos fibers, acts as a barrier to evaporative cooling. Studies have shown that the heat generated inside a Tyvek suit during physical activity can be substantial, significantly increasing the risk of hyperthermia.
The NIOSH mask, while crucial for respiratory protection, can also add to the feeling of restriction and potentially increase the perceived exertion and discomfort.
Finally, dehydration, often a consequence of inadequate fluid intake during demanding work, further impairs the body's ability to regulate temperature.
THE PROACTIVE APPROACH
Given these significant risks, a proactive approach from supervisors is paramount. This isn't just about reacting to a heat stroke incident; it's about preventing it in the first place. Key proactive measures include:
Pre-Job Planning: Assess the environmental conditions, including temperature and humidity, before work begins. Schedule physically demanding tasks during cooler parts of the day.
Work-Rest Cycles: Implement mandatory and frequent short breaks in cooler, shaded areas. These breaks must be enforced, not just offered.
Hydration Strategies: Ensure workers have access to ample cool water or electrolyte-containing beverages. Encourage frequent sipping, even if they don't feel thirsty. Educate them on the importance of hydration before, during, and after work.
Acclimatization: Gradually introduce workers to the hot work environment, allowing their bodies to adapt over several days.
Buddy System: Implement a system where workers monitor each other for signs and symptoms of heat illness, such as excessive sweating or lack thereof, dizziness, nausea, headache, confusion, and rapid heartbeat.
Training and Education: Provide thorough training on the risks of heat stroke, its signs and symptoms, and preventive measures. Workers need to understand the dangers and their role in staying safe.
Modification of PPE: Where feasible and without compromising safety, explore options like ventilated suits or cooling vests during periods of extreme heat.
THE HEAT STROKE PROTOCOL
Despite the best proactive measures, heat stroke can still occur. Therefore, a clear and well-rehearsed heat stroke protocol is essential:
Immediate Recognition: All supervisors and workers must be trained to recognize the signs and symptoms of heat stroke.
Rapid Cooling: If heat stroke is suspected, immediate and aggressive cooling is critical. Move the affected worker to a cool, shaded area. Remove outer clothing, including the Tyvek suit and mask. Apply cool water or ice packs to the neck, armpits, and groin. Fan the worker vigorously.
Activation of EMS: Immediately call for Emergency Medical Services (EMS). Heat stroke is a medical emergency requiring professional intervention. Do not delay calling EMS to attempt cooling alone.
Continued Cooling: Continue cooling efforts until EMS arrives.
Documentation: Thoroughly document the incident, including the timeline of events, environmental conditions, and actions taken.
COMORBIDITIES / SECONDARY DIAGNOSIS
Finally, it's important to be aware of other concurrent diseases and pathologies that can exacerbate the risk of heat stroke. These include:
Cardiovascular disease: Impairs the body's ability to circulate blood effectively for cooling.
Diabetes: Can affect hydration levels and thermoregulation.
Obesity: Increases metabolic heat production and reduces heat dissipation.
Certain medications: Some medications, such as diuretics and beta-blockers, can interfere with the body's ability to regulate temperature.
Age: Both very young and older workers are more susceptible to heat illness.
Supervisors must be aware of these potential underlying conditions and encourage workers to communicate any relevant health concerns.
In conclusion, heat stroke is a serious threat to asbestos abatement workers. By understanding the pathophysiology, implementing robust proactive measures, establishing a clear heat stroke protocol that includes immediate EMS activation, and being mindful of concurrent health conditions, we can significantly reduce the risk and ensure the safety and well-being of everyone on the job site. Let's make heat safety a priority, every single day.
References:


Comments