Is That Anxiety Really Just Stress? The Surprising Link Between Microbes and Your Mental Health
- OliveHealth

- Aug 7
- 3 min read
by Dr. Ed Fuentes

For centuries, we've grappled with the mysteries of the mind. From blaming demonic possession to focusing solely on brain chemistry, our understanding of mental illness has evolved dramatically. But what if tiny, often unseen, invaders play a much bigger role than we realize?
A fascinating recent review dives deep into the association between microbes and mental illness, and the findings are truly eye-opening. Forget just blaming stress or genetics – this research suggests that infections, both past and present, could be significant contributors to a wide range of psychiatric conditions.
A Historical Journey: From Witchcraft to Scientific Inquiry
Think back to the times of witch hunts and asylums. The article highlights how early beliefs attributed mental illness to the supernatural. It wasn't until the 19th century that the concept of mental illness as a disease of the brain began to take hold.
The early 20th century saw a controversial theory emerge – the idea that hidden infections were the root cause of mental disorders. While the extreme treatments that followed were tragically misguided, they hinted at a biological connection beyond just psychology.
The true turning point came with the discovery that syphilis, a bacterial infection, could directly cause severe psychiatric symptoms. The fact that treating the infection could alleviate the mental illness provided undeniable proof: microbes can impact our minds.
The Modern Picture: A Complex Web of Interactions
Fast forward to today, and research is uncovering a complex web of interactions between our bodies, the environment, and the microscopic world within us. This review highlights how a vast array of microbes – from bacteria and viruses to parasites and fungi – have been linked to conditions like:
Autism Spectrum Disorders
Schizophrenia
Bipolar Disorders
Depressive Disorders
Anxiety Disorders
Even Suicidality and Aggressive Behaviors
Think about Lyme disease, toxoplasmosis, herpes viruses, and even the more recent spotlight on SARS-CoV-2 (the virus behind COVID-19). The review meticulously lists a multitude of infectious agents and their potential connections to various mental health challenges.
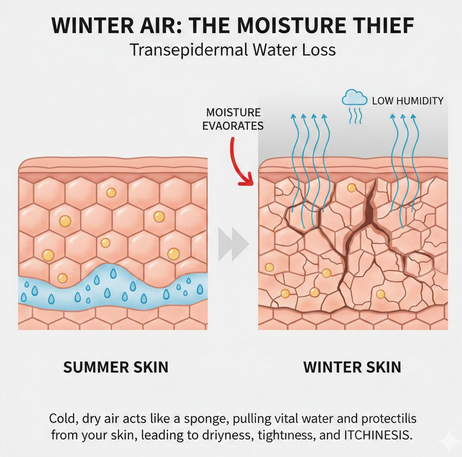
It's Not Just the Infection Itself
It needs to be emphasize that the impact of microbes isn't always direct. Sometimes, it's our body's reaction to the infection that causes problems. Chronic inflammation, autoimmune responses where the body attacks its own tissues (including the brain), and disruptions in crucial brain chemical pathways can all be triggered by infections, even ones we might not actively be aware of.
Why Haven't We Heard More About This?
There are several significant hurdles hindering progress in this field:
Lack of Awareness: Many mental health professionals have limited knowledge of infectious diseases, and vice versa.
Complex Interactions: It's challenging to study how multiple infections and other environmental factors interact with our individual biology.
Limitations in Testing: Current lab tests aren't always equipped to detect subtle or persistent infections.
Siloed Thinking: The medical field often operates in separate silos, preventing the necessary collaboration between specialists.
A Call for Change: Towards a More Holistic Understanding
This review isn't about blaming all mental illness on germs. Instead, it's a powerful call for a more holistic and integrated understanding. By recognizing the potential role of microbes, we can:
Expand Research: Investigate these connections further to uncover new pathways and potential treatments.
Improve Collaboration: Encourage psychiatrists, infectious disease specialists, and immunologists to work together.
Educate Professionals: Equip healthcare providers with the knowledge to consider infections in their assessments.
The Bottom Line: Could Your Mental Health Be Linked to a Hidden Infection?
While more research is undoubtedly needed, this review provides compelling evidence that the microbial world could be a missing piece in the puzzle of mental illness. It encourages us to think beyond traditional models and consider the possibility that infections, past or present, might be contributing to our mental well-being.
This doesn't mean you should panic and assume every mental health issue is an undiagnosed infection. However, it does suggest that a broader perspective, one that includes the potential impact of microbes, could lead to more effective diagnoses and innovative treatments in the future.
What are your thoughts on this connection? Share your comments below!
Disclaimer: This blog post is a summary of a scientific review and should not be taken as medical advice. If you are experiencing mental health concerns, please consult with a qualified healthcare professional.
References:
O’Connor, S.M.; Taylor, C.E.; Hughes, J.M. Emerging infectious determinants of chronic diseases. Emerg. Infect. Dis. 2006, 12, 1051–1057. [Google Scholar] [CrossRef] [PubMed]
Munjal, S.; Ferrando, S.J.; Freyberg, Z. Neuropsychiatric Aspects of Infectious Diseases: An Update. Crit. Care Clin. 2017, 33, 681–712. [Google Scholar] [CrossRef] [PubMed]
Bransfield, R.C.; Cook, M.J.; Bransfield, D.R. Proposed Lyme Disease Guidelines and Psychiatric Illnesses. Healthcare 2019, 7, 105.
Fallon, B.A.; Madsen, T.; Erlangsen, A.; Benros, M.E. Lyme Borreliosis and Associations with Mental Disorders and Suicidal Behavior: A Nationwide Danish Cohort Study. Am. J. Psychiatry 2021, 178, 921–931.


Comments